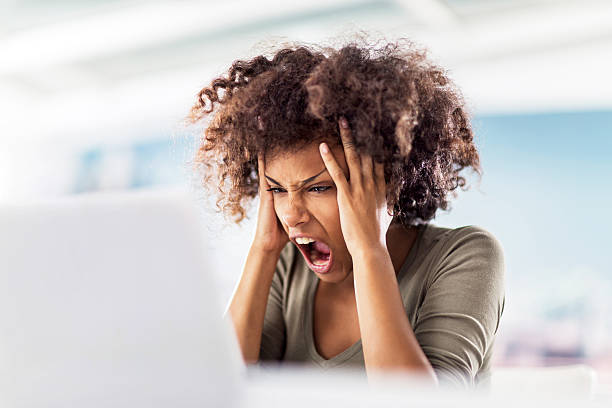
If you are here, I assume you’re struggling with Vulvodynia, it is ruining your life and don’t know what else to do. You’ve probably had countless doctor’s appointments, seen a variety of specialists, maybe tried acupuncture, numbing cream, antidepressants, anticonvulsant drugs, physical therapy, psychological therapy, maybe energetic healing. You may start to feel helpless living in pain, and that is completely natural when we cannot find answers or relief, you feel that Vulvodynia is ruining your life, and all you can do is continuously look for answers online as you aren’t getting enough from the professionals you’ve seen so far.
I know the struggle very well. I spent countless hours reading online people’s experiences, researching what it is that happens in our bodies for this pain to happen, and tried every treatment I could come across. Not only did none of this help, but it also gave me crippling anxiety. I read about cases of women who had it for years, women that had to stop working because of it, and every bad story that just kept messing with my mental health more and more. As a start, I’d like to say to you: don’t continue looking for hope on forums. If you find good platforms, yes, that’s great! Unfortunately, I have to tell you what you will find is going to be very little hopeful, because it is biased. The bad will override the good.
Going back to tell your story, even if it’s a happy ending one, can be very vulnerable
When women heal, they want to leave this chapter of their lives in the past. They don’t go back online and tell their success story, at least not in most cases. So you will find much more negative information than positive. This will affect how you feel, it will cause more anxiety, it will make you obsess more over it and as a result, make the pain worse. Now you are reading this, so please make this your last stop. Yes, you can heal, yes many of us have. No, not all of us go back and tell our story, and I include myself in it for some time. And why? Well, the pain in itself is traumatic. The place it may stem from is traumatic (at least in my case it was very related to sexual abuse), but healing from vulvodynia in itself, is traumatic too. You encounter multiple specialists that don’t know what happens to you, they don’t even know the name of it. I kept going from one doctor to another, to all alternative therapists I could find, to psychotherapists, physical therapists… At some point, I was so tired of telling my story over and over to find no answers, that I felt I couldn’t do it anymore. Eventually, I started crying every time I went into a new specialist’s office. I couldn’t gather the strength to keep telling anyone about my pain just to be given a variety of useless “solutions”, if any at all. Finding hope in this was extremely difficult.
“Feeling this isolated in my pain without answers, broke me down even more”
It felt like there was a huge burden on me, not letting me breathe. I dreamt of the pain, no matter what I did during the day, I kept feeling the pain, I missed out on meeting with friends because of it… I stopped my whole life and it was me and the pain in a dark hole. It was horrible, lonely, painful, heartbreaking. Vulvodynia literally was literally ruining my life, and I was only in my early-mid 20s. So when I started to improve and when I eventually healed… I didn’t want to look back. I didn’t want to live over all of that. I didn’t want to hear the word Vulvodynia ever again. And this is the case for many, many women. When we heal, we are SO done with it, that we just want to forget about it. Not out of a place of selfishness, it is not that we don’t want to bring hope to others, it is just that we are exhausted mentally and physically from it.
I wanted to help others heal from Vulvodynia, but then…
It is “funny” because when I had my pain I was a psychology student, and I thought I would heal from it and then help others out of it. But there was an impasse of time, where I was almost fully healed, where I didn’t want to hear about vulvodynia anymore. It had been such a long journey, and I couldn’t see myself poking that wound anymore. I was still vulnerable, it had been a lot of work, I was sensitive, and still very wounded only from the healing journey alone. I thought vulvodynia was a chapter of my life I didn’t want to remember ever again. I wanted to leave those memories buried as far as possible from it. While through my own healing I knew I wanted to work with a mind-body approach in psychotherapy, I couldn’t bring myself to look at the V word anymore. But, once I was already more stable and I could look back, I could see all the pain and despair I felt, and I knew there were more women who needed answers.
It wasn’t easy to get into this work, and sometimes it still stirs things in me
I was still hesitant when I signed up to work with some of the specialists that contributed to my healing, and to this day, things still stir up inside of me when I speak about it. But I know that through this work, I can bring the solutions I wish I had more readily available. So I learned everything I could – and I am still in constant learning, training, and expanding my knowledge – to bring the answers it took me years to find. I love psychology and somatic work, however, it was not enough to address everything that is needed to heal from vulvodynia. There are bits of it that I really enjoy, other ones that are not so enjoyable. While the good overrides the downside, through my clients I remember all too well my own struggle… and it still feels tender. Even writing about it, still takes me back to days spent in bed and completely misunderstood, it is not pleasant, but I shared my story because I decided to take this as part of my purpose and apply it to my work. Otherwise, I probably wouldn’t go into this much detail, if any at all. But because I decided to continue with my mission on helping others and I made this part of my work, now I speak so much more about vulvas and Vulvodynia, but the truth is, that if I had been an accountant, or a baker, or something else that has nothing to do with health… I probably wouldn’t be speaking about Vulvodynia. Maybe AT ALL. Because it’s painful. Because we all wanna forget about it. Because it’s daunting. Because it took so many years of my youth and vitality away.

What you’ll find in forums, is much more pain than hope
So please hear me in this, don’t think everything you see online is an accurate depiction of the numbers of people who healed. It is just that most women, once they do, they never look back. They want to forget how traumatic this all has been and I cannot blame them for it. But I don’t want you to look at all the stories and think that this will be the rest of your life. It doesn’t have to be. With all the sorrow of my heart, that is someone’s situation, but we cannot tell ourselves we are doomed, or else our brain will pick up on it.
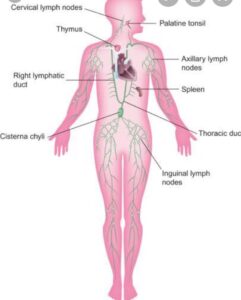
Our body is listening to our beliefs, allow it to believe it can heal
Our nervous system and body are always eavesdropping on our beliefs. If you believe you cannot heal you most likely won’t. If you believe your body can heal, it will. And yes, I know the amount of doubt you carry with you right now. I did too! I know the hesitation, the “ I have had this for too long, how will it go away”, or the “I haven’t found anything that truly helps yet”… but that is just a “yet”. I clang onto hope like grasping for straws. For as little as it could be, I kept it with me. I kept going and even though I tried to make peace with the situation, I didn’t resign myself to it. Making peace doesn’t mean giving up, it just means letting go of resistance. So the number one advice I would give to anyone going through pain right now is don’t compare your experience to others. As Sean Stephenson said: “Never believe a prediction that doesn’t empower you.”
Don’t obsess over the pain fluctuations
If you are going to take other people’s experiences as your prognostic, take one of those who have healed. Tell your mind, your body, and your spirit, that you are healing. That others have done it before you, and therefore you can too. Stop being hypervigilant about Vulvodynia. Some days will be better, some days will be worse. Even if you have a flare it doesn’t mean it’s gonna stay worse. It will come back to the “baseline” pain. And eventually, it will get better too. The more you obsess over the pain, the more you’re feeding it. While stopping to think about it is difficult, don’t do it more than you should. You don’t need countless hours in front of the computer reading about it.You don’t need to constantly gaze at your vulva unless it is to tell it how beautiful it is. You don’t need to worry you will do something “you shouldn’t” and make it worse. Do what’s on your hands to reduce the amount of attention you give it, so your mind has other things to entertain and gives you more of those, instead of the one (the V) that you’re focused on.
Long story short, in order to re-train yourself to not feel pain, minimize the actions that feed it. While it is difficult to stop thinking about it, you can choose to watch a comedy instead of reading people’s experiences for hours before bed. Increase the joy and decrease the amount of time you dedicate to your Vulvodynia. Your vulva will thank you 🙂


 Vulvodynia is an
Vulvodynia is an Pain is created in the brain
Pain is created in the brain



 I think we are headed in the right direction in normalizing speaking about it though, as some public figures are using their voice to bring awareness to some health conditions.
I think we are headed in the right direction in normalizing speaking about it though, as some public figures are using their voice to bring awareness to some health conditions. 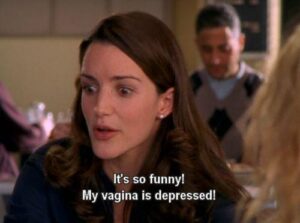

 Now, I am sure that this is not the case for everyone, and that there will be sufferers with a supportive family, friends, and close circles who care to listen to them and do their best to understand. That’s great and extremely helpful in the healing journey, however, it is not the norm. I had a few people close to me do their best to understand me, but not the majority. Most of us get tired of even speaking about it, even when we are unable to walk or do many other things because the pain is too strong. We give up because we know people won’t get it. They won’t care, it will be lost time and energy. So many times I’ve been mocked for my clothing choices and other things by my own family, not realizing
Now, I am sure that this is not the case for everyone, and that there will be sufferers with a supportive family, friends, and close circles who care to listen to them and do their best to understand. That’s great and extremely helpful in the healing journey, however, it is not the norm. I had a few people close to me do their best to understand me, but not the majority. Most of us get tired of even speaking about it, even when we are unable to walk or do many other things because the pain is too strong. We give up because we know people won’t get it. They won’t care, it will be lost time and energy. So many times I’ve been mocked for my clothing choices and other things by my own family, not realizing 
 Complete this form to send me a message. Everything submitted through this form is fully confidential and I will reach back out to you promptly.
Complete this form to send me a message. Everything submitted through this form is fully confidential and I will reach back out to you promptly.